Struggling to conceive is heartbreaking — even if you already have a child. You’re so grateful for the baby you have, but your family doesn’t feel complete, and it’s confusing to understand what’s changed. You might even feel like family, friends, and even your doctors are dismissing your concerns.
What you might not know is that secondary infertility is common, just like first-time challenges getting pregnant. Around 11% of people in the US who already have a child will struggle to conceive again. Let’s learn a little more about what causes secondary infertility, how it’s treated, and what you can do at home to improve your chances of getting pregnant.
What is secondary infertility?
Secondary infertility is the medical term for not being able to get pregnant or carry a baby to term after the birth of one or more children. To qualify as secondary infertility, your previous births must have occurred without help from fertility medications or treatments.
Similarly to primary infertility, you should visit a healthcare provider if you’re younger than 35 and have been trying to conceive for a year or if you’re older than 35 and have been trying for six months.
What causes secondary infertility?
Secondary infertility can be affected by both male and female factors.
Secondary infertility can be caused by:
- Age related egg quality issues
- Irregular or lack of ovulation caused by PCOS
- Low sperm quality
- Tubal issues
- Inflammation or scarring from endometriosis
- Complications from a past pregnancy
- Other uterine conditions like uterine fibroids or adenomyosis
- Lifestyle factors, especially large shifts from your past pregnancy, including smoking, excessive alcohol consumption, significant weight gain, exposure to environmental pollutants and toxins, or certain medications
About one in five people experiencing secondary infertility will be diagnosed with unexplained infertility. This is when fertility testing hasn’t found a cause for why you can’t get pregnant. And while it should be good news that your scans and labs are all coming back normal, it can also be extremely frustrating not having a reason why you can’t conceive. If you have been told you have unexplained infertility, ask your doctor what the possible explanations could be.
Can a C-section cause secondary infertility?
Around 20% of people who give birth via cesarean section have difficulties getting pregnant with a second child. In some cases, c-sections can lead to a defect in the area of the scar called an isthmocele. This defect can make it harder to conceive.
During your fertility evaluation, your doctor will perform an ultrasound to determine whether you have a cesarean scar defect that needs repair by a minimally invasive gynecologic procedure.
How is secondary infertility diagnosed?
The tests your fertility specialists will use to diagnose secondary infertility are similar to what is used for primary infertility. You’ll begin with a physical exam and a thorough health history. Your doctor will then use one or more of the following tests or procedures:
- Semen analysis to determine the number, morphology, and motility in a sample
- If sperm quality is poor, a referral should be made to a reproductive urologist who will perform a Male physical examination to determine if any testicular abnormalities are present and to run hormone and genetic tests when appropriate.
- Ovarian reserve assessment, including measuring the level of Anti-Mullerian Hormone (AMH) and Follicle-Stimulating Hormone (FSH) in the blood
- A hysterosalpingography or HyCoSy with Exemview to view the structure and function of the uterus and fallopian tubes
- Pelvic ultrasound to identify uterine fibroids, polyps, or any other structural abnormalities
Depending on your condition, additional tests may be needed to determine the cause of infertility.
How is secondary infertility treated?
The treatment for secondary infertility is largely the same as what is offered for primary infertility. Your fertility specialist will tailor your treatment to your specific needs and circumstances, but your plan may include:
Medications
Your doctor may prescribe medications that stimulate ovulation, such as Clomid or Gonadotropin, in combination with fertility treatments like intrauterine insemination (IUI) or alone. These medications can help balance hormone levels and improve the chances of ovulation and conception.
Surgery
For certain conditions, such as blocked fallopian tubes, scar tissue, or a defect in the uterine scar from a C-section, surgery might be recommended to repair what’s complicating the reproductive process. Surgical interventions can often resolve physical issues, potentially restoring fertility and increasing the likelihood of a successful pregnancy.
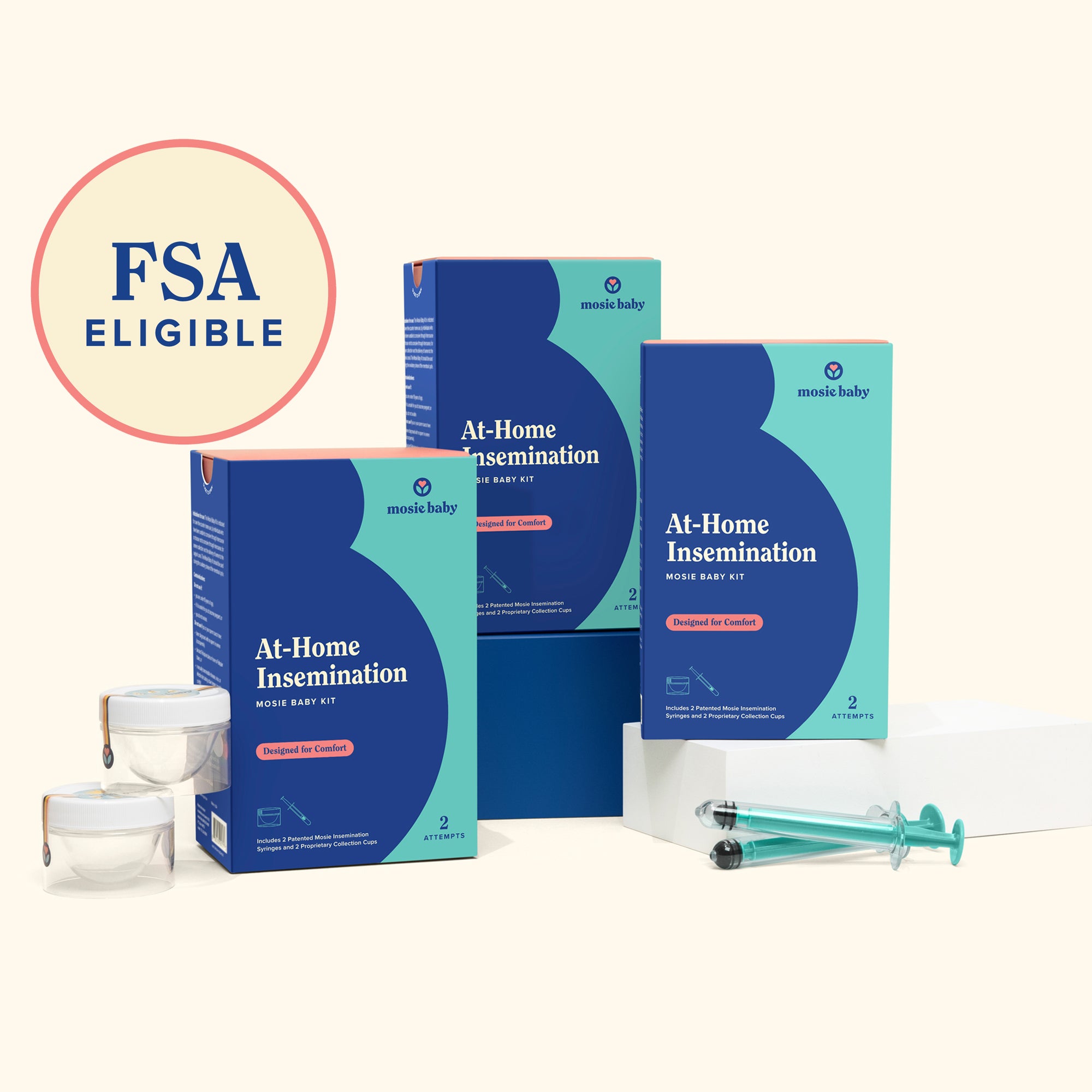
Intravaginal Insemination (IVI)
IVI, although not a fertility treatment, is a simple, at-home option you can use to try to conceive that involves placing sperm inside the vagina, near the cervix, using a syringe. The entire process can easily be done in the comfort and privacy of your own home without needing a doctor or midwife. IVI is a great way to take the pressure off having to time intercourse. It's also a wonderful alternative to try if you're experiencing performance anxiety, dealing with unexplained infertility or sexual dysfunction, facing mild male fertility challenges, or using donor sperm.
The Mosie Baby At-Home Insemination Kit is the first FDA Cleared at-home IVI kit. The Kit includes 2 attempts with 2 Mosie syringes featuring a patented nub tip with a unique slit opening. The Mosie Baby Kit is not intended to treat infertility.
Intrauterine Insemination (IUI)
IUI is a procedure that involves placing sperm inside the uterus using a catheter. Before this, the sperm gets a little prep — it’s washed and concentrated to increase the chances of fertilization. Most of the time, IUI is performed by a fertility specialist. However, there are some midwives who offer this service. IUI is often used in cases of mild male factor infertility, unexplained infertility, or when there are cervical issues. It's a less invasive and expensive option compared to IVF and is often used when simpler methods have not been successful.
In Vitro Fertilization (IVF)
IVF is a bit more involved than IVI and IUI but is a very effective fertility treatment. The process involves retrieving eggs from the ovaries after a round of hormones to stimulate ovulation. The eggs are then fertilized by sperm in a lab and transferred back into the uterus. IVF is used to treat a range of fertility challenges, whether it’s more complex male fertility issues, blocked fallopian tubes, or factors related to age. The process is more invasive and expensive than other options, but it also generally has a higher success rate. To learn more about IVF you can sign up for a class here.
What can I do at home to improve my chances of getting pregnant before I see a fertility specialist?
Living in the waiting zone before you officially qualify for fertility treatment can be one of the most painful parts of this journey. You’re trying to convince yourself to calm down and relax, but the worry builds every time you see another negative pregnancy test. Thankfully, there are things you can do at home to positively impact your fertility and health before you hit the one-year or devastating third loss mark.
Track your cycle
If you aren’t doing so already, start tracking your cycle. Knowing when you’re ovulating is the key to getting pregnant. It’s also helpful to bring your cycle history to your fertility specialist so they have more information about your body from the start.
If you’re finding it difficult to identify your fertile window — the short period of time when you’re able to get pregnant — using an ovulation predictor kit (OPK) can be helpful to pinpoint the best time to try to conceive.Ovulation predictor kits are also extremely helpful for people with irregular cycles to time intercourse.
There are lots of ways to determine when you’re ovulating, including using fertility awareness-based methods like cervical mucus tracking or the position of your cervix. The Kegg is an innovative fertility tracker that senses cervical fluid and tells you when you’re most likely to conceive.
Find out if you’re ovulating
If you’re using an OPK to monitor your hormones and find your fertile window — there’s one thing you should know. To signal your ovary to release a mature egg, your brain releases a spike in luteinizing hormone. However, sometimes, your ovary doesn’t listen, and an egg isn’t released. So while OPKs measure the level of LH in your urine, an at-home ovulation test like the Proov Confirm can help to confirm whether or not you actually ovulated by measuring the amount of PdG in your urine.
If you aren’t ovulating, we encourage you to speak to your doctor as soon as possible to determine any underlying causes and start the right treatment for you.
Lifestyle changes
Healthy lifestyle changes will be an important part of your infertility treatment, so it can’t hurt to start them early. Your doctor may recommend the following in order to improve your fertility:
Begin taking a prenatal vitamin
Prenatal vitamins are a great way to give your body a boost while trying to conceive!
Quit smoking and limit alcohol consumption
Smoking has been shown to significantly reduce fertility in both males and females, and it can also impact the success rates of fertility treatments. Similarly, alcohol consumption has been linked to a greater than 50% reduction in the chances of conception during a menstrual cycle.
Improve your nutrition
A diet high in trans fats, refined carbohydrates, and added sugars can negatively affect fertility, causing ovulation disorders, including increasing the risk of PCOS. Making the switch to a diet rich in fiber, omega-3 fatty acids, plant-based protein, and vitamins and minerals, like the Mediterranean diet, has been shown to improve fertility.
Balance your blood sugar
Insulin is a hormone that helps manage your blood sugar levels. It also affects a protein called sex hormone-binding globulin (SHBG), which controls the levels of sex hormones in your body. In people with PCOS, when insulin levels are too high, SHBG levels can decrease. This drop leads to hormonal imbalances, affecting how the ovaries function.
Even if you don't have PCOS, high insulin levels can still impact your reproductive health. They can disrupt normal ovarian function and hormone production, leading to irregular ovulation.
To balance your blood sugar, focus on a diet with fewer processed foods and those high in sugar and refined carbs. Include more whole foods, like vegetables, fruits, whole grains, and proteins. Regular physical activity is also crucial in maintaining healthy blood sugar levels.
Manage your stress
The relationship between stress and infertility is controversial. High-stress levels can impact fertility by disrupting hormonal balance and potentially interfering with ovulation and sperm production.
To reduce stress, consider engaging in relaxation techniques like yoga, meditation, or deep breathing exercises. Regular physical activity, maintaining a healthy diet, getting adequate sleep, and seeking support through counseling or support groups can also help manage stress levels effectively.
Trying to conceive with secondary infertility
Struggling to grow your family when you’ve already had a baby can be a rollercoaster of emotions, and it’s normal to feel frustrated or confused. But, with the right support and treatment, many people find a way to conceive again — even if it takes longer than you’d hoped.
The important thing to remember is that you know your body, and you don’t need to wait to take proactive steps to support your fertility. Tracking your cycle, adopting healthy lifestyle choices, or trying IVI are great ways to give yourself a headstart to try to conceive. We’re rooting for you every step of the way and hope you find the path that works for you soon.
Resources
Advances in Nutrition. (2021). Female Fertility and the Nutritional Approach: The Most Essential Aspects. Retrieved from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8634384/
AIChE. (2017). Detection of ovulation, a review of currently available methods. Bioengineering & Translational Medicine. Retrieved from:https://aiche.onlinelibrary.wiley.com/doi/10.1002/btm2.10058
Dialogues in Clinical Neuroscience. (2018). The relationship between stress and infertility. Retrieved from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016043/
Human Reproduction. (2020). Post-Caesarean section niche-related impaired fertility: hypothetical mechanisms. Retrieved from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7568911/
Reviews in Obstetrics and Gynecology. (2008). Diagnosis and Treatment of Unexplained Infertility. Retrieved from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2505167/
Science Direct. (2021). Female Fertility and the Nutritional Approach: The Most Essential Aspects. Retrieved from:https://www.sciencedirect.com/science/article/pii/S2161831322005129#:~:text=Infertility%20is%20an%20increasing%20problem,sugars%20can%20negatively%20affect%20fertility.